Craig Settles: Communities to Roll Out Telehealth Integration
‘We figured out how to train people to be digital navigators [and] get customers comfortable with telehealth.’

A pacesetter among municipal broadband owners, the City of Chattanooga is giving away 1,000 free telehealth appointments that also brings broadband into low-income homes. Vistabeam, a Nebraska Wireless ISP, is bringing telehealth to rural towns through Community Empowerment Centers that increase broadband as well as improve residents’ health.
“The Enterprise Center works hard at the intersection of technology and inequality, whether it’s using technology to work efficiency, for learning, or improving personal health,” states CEO Deb Socia. The center is partnering with residents, community organizations and the Parkridge Medical System to identify needs and bring in resources to combat high levels of diabetes, stroke, heart disease, and asthma.
Vistabeam owner Matt Larsen says, “You can’t just lay down some fiber and routers, then call this a broadband success. Rural areas often lack the human and tech resources necessary for broadband to thrive.” So Vistabeam is designing Community Empowerment Centers to offer communities private telehealth consultation rooms, digital skills and telehealth training, full-time digital navigators and inventory rooms with shared computing devices and equipment.
These and other communities are finding that telehealth increases broadband adoption as well as improves the physical and economic health of residents. Telehealth is the “killer app” that can harness and focus broadband investments into digital inclusions advancements for urban and rural communities.
A perfect storm for telehealth
Chattanooga’s public broadband network, through a city electric power board that offers both electricity and broadband, is an advantage to telehealth. Socia says, “EPB has a deep connection to the community, and they invest money, technology in public spaces, and energy upgrades in the homes. EPB cares about the health of our community.” (EPB, formerly known as the Electric Power Board of Chattanooga, provides broadband in the city.) Communities without public broadband may have to work harder to find large ISPs with similar levels of commitment.
Communities wanting to leverage telehealth likely will need new strategies for winning and managing grants. You can’t have telehealth without broadband, but the integration of broadband to facilitate telehealth delivery may involve a myriad of people, organizations, and resources besides the network builder.
For years Chattanooga has had a culture of cooperation among its many civic groups. The nonprofit Orchard Knob had a preexisting collaborative, so when the telehealth opportunity came up as part of a larger “healthy community” initiative, it was it much easier to create a grant of the size that the group currently has.
The community created the Orchard Knob Collaborative, which includes Parkridge Medical Center with their 1000 telehealth appointments, the Orchard Knob Neighborhood Association, Habitat for Humanity of Greater Chattanooga Area and United Way of Greater Chattanooga. EPB contributed money, energy upgrades, and public WiFi. Green Spaces is another nonprofit and the Center provides project management plus various Tech Goes Home digital inclusion programs.
Telehealth opens the door for larger grants. “I think the anticipated grant-raising outcomes are quite specific when you’re producing social determinants of health,” Socia says. “Projects that involve telehealth are a much tougher ‘ask’ for funders and everyone else involved. But at the same time, you can leverage other additional dollars and other partners for a much better healthcare outcome.”
Telehealth and the ‘human element’
Every state is developing a digital equity plan. How important is telehealth to the success of a digital equity plan? Quite important! But remember that telehealth deployment strategy in rural communities likely could take shape differently than urban deployment. Vistabeam’s Centers represent one approach.
Digital equity in telehealth is just one component of a giant ecosystem of social services that good societies use to help take care of people. The challenge is the need to successfully coordinate scarce resources to get maximum impact from the resources. However, in rural communities there can be a real lack of coordination between a lot of these resources.
“It makes sense to start out by focusing on getting telehealth into some smaller communities at locations where people can come in and access telehealth in an environment that develops trust and familiarity with the technology,” says Larsen. “To do that, we’re going to need a ‘human element’, facilitators such as digital navigators to plug community telehealth into the ecosystem. A lot of rural communities have trust issues with government programs.”
Using surplus office space to create customer service centers
There are plenty of large incumbents’ mobile device showrooms in communities. But these employees tend to be sales-oriented with scripted content. Vistabeam happens to have surplus office space they are using to create true customer service centers.
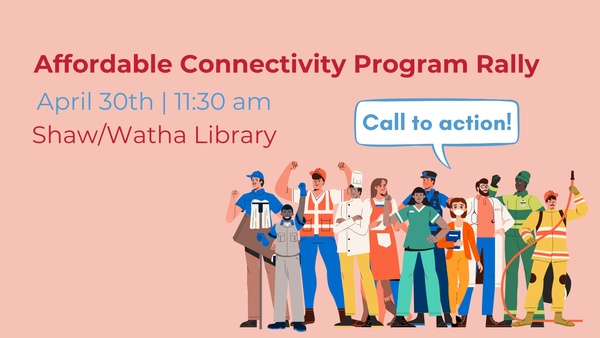
“We figured out how to train people to be digital navigators, we get customers comfortable with telehealth and our staff connects people with complementary social services and other resources,” says Larsen. For the last few months, Vistabeam has been promoting exclusively the FCC’s Affordable Connectivity Program of free Internet access and subsidized computing devices. There’s a complex enrollment process residents have to complete that’s confusing for many, so Vistabeam trained staff to walk people through the process, get them qualified, and connected.
As for the potential of telehealth deployment to the home, Larsen believes the technology represents a tremendous amount of potential utility and value for both rural and urban broadband deployments. Though broadband is currently underutilized for telehealth, in large part because communities are just beginning to plan for it, the pandemic revealed a burning need for strong video streaming capacities to bridge doctors and patients.
“What’s missing is a telehealth killer app or device,” says Larsen. “I believe preventive healthcare will be the answer – technology that detects or prevents things from happening before they become big problems. This app could be a way to check vital statistics and watch for health or illness markers. Maybe we’ll see a device connected to the Internet that accesses research data to help you and your health professional with health planning.”
Just about everybody gets sick or hurt, or they are responsible for others when those loved ones aren’t doing well. Telehealth and its many iterations are designed for people to use when they’re sick or hurt or for preventative healthcare. The universality of telehealth and its symbiotic relationship with broadband technologies give communities great potential for expanding digital inclusion. Together with the bezillion grant dollars coming out the ying yang, what we’re seeing is the perfect digital storm.
Craig Settles conducts needs analyses, planning, and grant assessments with community stakeholders who want broadband networks and telehealth to improve economic development, healthcare, education and local government. This piece is exclusive to Broadband Breakfast.
Broadband Breakfast accepts commentary from informed observers of the broadband scene. Please send pieces to commentary@breakfast.media. The views reflected in Expert Opinion pieces do not necessarily reflect the views of Broadband Breakfast and Breakfast Media LLC.